Medical 3D printing applications
This article will discuss the requirements within the medical industry that make AM an ideally suited technology for many applications.

Introduction
At a rapidly growing rate, the medical industry continues to recognise the added value of additive manufacturing (AM or 3D Printing) for a vast range of medical applications. AM is now used in the development of new surgical cutting and drill guides, orthopedic implants, and prosthetics as well as the creation of patient-specific replicas of bones, organs, and blood vessels.
A study by Wohlers in 2015 revealed that 13% of all 3D printing revenue comes from companies who are linked to the medical industry. More than 20 different implants ranging from cranial implants to hip, knee, and spinal implants approved by the Food and Drug Administration (FDA) are produced with various AM technologies. Furthermore, to date, more than 100,000 acetabular (hip cup) implants have been produced via AM with approximately 50,000 of them implanted into patients.
All of these milestones continue to reinforce the important role AM now plays in the medical industry where custom products tailored to each individual can be manufactured. This improves medical professionals understanding of patients (see Surgical learning tools) and improves patient comfort level by allowing interaction with products that are designed specially for their anatomy.
This article will discuss the requirements within the medical industry that make AM an ideally suited technology for many applications and present the most common methods of data generation for the production of 3D medical models. Common medical industry applications will also be discussed along with the limitations and restrictions AM must overcome to further impact this industry. Finally, a series of case studies that have made use of AM in the medical industry will be presented.

Medical industry requirements
Customisation
The individualized nature of health care means that AM is an ideal solution for the medical industry. Rather than manufacture thousands of identical components, AM enables the creation of prosthetic and orthotic devices tailored to a patient’s specific anatomy improving their effectiveness.
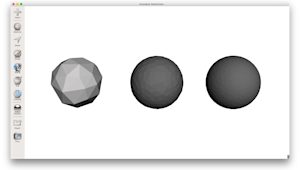
Complexity
Where in the past, traditional manufacturing may have struggled to create complex, organic shapes, the designs that AM technologies are now able to print are potentially limitless. Thin scaffolds that perfectly follow the contour of a bone or porous metal parts are easily manufacturable opening the door to many applications and designs that were not previously possible (including facial bones, radius and ulna).
Lead time
Lead times to create tooling, whether in-house or outsourced, can be lengthy and expensive. One of the hallmarks of AM is that is provides designers and engineers the tools to quickly create and iterate designs, communicate more effectively using realistic prototypes and ultimately reduce time to market. An essential part of the success of any medical device is the feedback from physicians and patients and the speed these design improvements can be implemented at. Within a matter of hours it is now possible to iterate the design of a medical tool based on direct feedback from the surgeon who will use it and print a new prototype for evaluation. The fast feedback loop accelerates design development. Manufacturers can also use early AM parts to support clinical trials or early commercialization while the final design is still being optimized.
Cost
As well as the ability to create custom, complex components, AM is best suited for low volume production meaning cost often drops while effectiveness increases. The individual nature of production means expensive tooling or machining processes are no longer required. AM technologies also only produce parts using the material they need reducing waste and further reducing costs.
Multi-material prints
Some AM technologies are now also able to print 3D models from different materials in a single print procedure. The advantage to this is that a model can now have different sections representing bone, organs and soft tissue allowing surgeons and physicians an even greater understanding of how a patient’s body will feel when using a model to practice for surgery or for educational purposes.
Sterilizability
Due to the application of some parts used in the medical industry, sterilizability is an important material property. A list of some of the most common sterilizable materials used in AM are shown in the table below.
| Material | Technology | Acceptable sterilization method |
|---|---|---|
| ABS M30i | FDM | Gamma irradiation, ethylene oxide |
| PC-ISO | FDM | Gamma irradiation, ethylene oxide |
| PPSF | FDM | Steam autoclave, ethylene oxide, gas plasma, chemical, gamma irradiation |
| Ultem | FDM | Steam Autoclave |
| PA12 (nylon) | SLS | Steam autoclave, ethylene oxide, gas plasma, chemical, gamma irradiation |
| 17-4PH Stainless Steel | DMLS/SLM | Steam autoclave, ethylene oxide, gas plasma, chemical, gamma irradiation |
Data generation (CT, MRI, 3D scan)
The ability to produce patient-specific parts directly from scan data is an obvious benefit that is not cost-effective with most conventional manufacturing techniques. These tailored parts are made possible through software that converts the patient’s own scans (using techniques like computerized tomography (CT), magnetic resonance imaging (MRI) and laser scanning) into 3D files. These files essentially encode each patient’s specific anatomic or pathologic features, which then can be fabricated by 3D printers.

CT - CT uses many x-ray projections through a subject to computationally reconstruct a cross-sectional image. CT is considered the imaging methods of choice for bone imaging and for the collection of data that is then used to produce medical models of hard tissue structures like bone. CT scans are widely used in emergency rooms because the scan takes fewer than 5 minutes. Because patients are exposed to small amounts of radiation CT scans can sometime be unsuitable.
MRI - MRI makes use of a very powerful magnet to align the nuclei of atoms inside the body, and a variable magnetic field that causes the atoms to resonate, a phenomenon called nuclear magnetic resonance. The nuclei produce their own rotating magnetic fields that a scanner detects and uses to create an image. Differences between normal and abnormal tissue are often clearer on an MRI compared to a CT scan. Typically MRI scans also take longer to complete.
Laser scanning - Laser scanning scans the surface of an object and captures data represented as a collection of points (a point cloud), which is then be used to generate a 3D surface. This enables parts that would be very difficult to precisely measure and 3D model, to be digitized and accurately reproduced. Unlike CT or MRI scanning, laser scanning does not show the internal features of the object being scanned. Also, laser scanners come in a range of sizes for different applications with handheld variations available offering a large advantage over the industrial-sized CT and MRI scanners.
Common applications
Surgical learning tools
While much of the focus for 3D printing in the medical industry has been around implants and medical devices used by patients, one of the largest areas of application has concentrated on anatomical replicas. Historically, clinical training, education, and device testing have relied on the use of animal models, human cadavers, and mannequins for hands-on experience in a clinical simulation. These options have several deficiencies including limited supply, expense of handling and storage, the lack of pathology within the models, inconsistencies with human anatomy, and the inability to accurately represent tissue characteristics of living humans.

Physicians are now using models produced by AM from patient scan data to improve the diagnosis of illnesses, elucidate treatment decisions, plan, and, in some cases, even practice selected surgical interventions in advance of the actual treatments. The models help physicians understand patient anatomy that is difficult to visualize, especially when using minimally invasive techniques. Models also assist in accurately sizing medical devices. Physicians can also use the models to explain an upcoming surgery to patients and their families and to communicate the surgical steps to the clinical team.
To help reduce cost some facilities have developed procedures where surgeons practice and plan operations on low cost mannequins that are transplanted with with patient-specific AM models. This coupled with the fact that AM technologies are able to produce both hard and soft materials in a single part, allowing the accurate replication of human tissue, calcification, and bone, means that surgeons can now obtain an even better understanding of exactly how a procedure needs to be performed right down to the touch and feel of the different parts of a patient’s anatomy.
| Technology | Best suited for |
|---|---|
| FDM | FDM is ideal for geometrically basic surgical models that do not require a high level of detail or include intricate features. A large range of colors are available. Print layer lines will be visible. |
| SLA | Best suited for smaller models with a very smooth surface finish. Able to produce very intricate details and features. Colors are limited. |
| SLS | SLS can produce parts with very complex geometries and good strength. Parts are typically white with a matte-like grainy surface finish. Excellent for replicating bone. |
| Material jetting | The optimal solution for high detail, multi color, multi material prints. Can also produce transparent parts. Surface finish is very smooth and models can be larger in size than FDM or SLA. More expensive than other AM technologies. |
Surgical guides and tools
Much like a drill jig is used in manufacturing to ensure a hole is placed in the exact right location, physicians also implement guides and tools to assist in surgery. Historically, surgical guides and tools were generic devices made of titanium or aluminum. By implementing AM, physicians are able to create guides that precisely follow a patient’s unique anatomy, accurately locating drills or other instruments used during surgery. AM guides and tools are used to make the placement of restorative treatments (screws, plates, and implants) more precise, resulting in better postoperative results.

Orthopedic surgeons and craniofacial (cranium and face) surgeons are one of the most regular users of AM guides and tools. In 2014, 23 custom surgical guides and templates were fabricated to assist partial or total knee replacement surgeries, more than 112 surgical guides were fabricated to assist various craniofacial surgeries and nine different titanium alloy Ti-6Al-4V craniofacial implants were surgically implanted into patients in Egypt alone. Surgical guides, derived from patient scans to precisely match their anatomy and made from PC-ISO (a sterilizable FDM plastic), are compatible with human tissue for short-term contact. This allows them to be placed against the patient’s anatomy for a more precise cut or drill hole.
Anatomical models (bone models) and surgical guides are also regularly both produced via AM and used collaboratively to plan and test the best locations for stabilizing screws or plates that conform to the patient’s bone surface before performing surgery.
| Technology | Best suited for |
|---|---|
| FDM | Multiple plastics available with some also sterilizable. FDM is low in strength but ideal for iterative, low-cost prototyping to optimize the design of a tool or guide. |
| SLS | Used for making functional guides and tools with similar strength to injection molded nylon. PA12 nylon is also sterilizable |
Implants
AM’s ability to produce fine mesh or lattice structures on the surface of surgical implants can promote better osseointegration and reduce rejection rates. Biocompatible materials such as titanium and cobalt– chrome alloys are available for applications in maxillofacial (jaw and face) surgery and orthopedics. The superior surface geometry produced by AM has been shown to improve implant survival rate by a factor of 2 when compared to traditional products. The porosity of these AM products coupled with the high level of customization and ability to manufacture them from traditional medical materials has resulted in AM implants becoming one of the fastest growing segments of the AM medical industry.

| Technology | Best suited for |
|---|---|
| Metal printing | Very high accuracy and strength and able to produce very complex geometries that accurately match to the contours of a patient's anatomy. Uses common medical metals (titanium and aluminium). Porous surfaces and intricate scaffolds are able to be printed. |
Prosthetics
In the United States alone, close to 200,000 amputations are performed each year, with prosthetics priced from $5,000-$50,000 replacement or alterations can be time consuming and expensive. Because prosthetics are such personal items, each one has to be custom-made or fit to the needs of the wearer. AM technology is now regularly being used to produce patient specific components of prosthetics that match perfectly with the user’s anatomy. The ability to produce complex geometries from a range of materials has resulted in AM being adapted at the locations where prosthetics are in contact with a patient. AM technology has been used to produce everything from prosthetic leg connections that fit comfortably onto a user through to a complex and highly customised facial prosthetic for a cancer patient.
AM is also being used in the manufacture of low-cost prosthetics. The collaborative nature of the AM industry has meant that a quick internet for 3D printed prosthetics reveals a huge range of peer-reviewed products that can be printed on desktop AM printers at a very low cost. These designs can easily be scaled or altered to perfectly match the size of the user. The e-NABLE Community comprises of a group of individuals from all over the world who are using their 3D printers to create free 3D printed hands and arms for those in need of an upper limb assistive device. Concepts like this are now becoming more commonplace as AM continues to move into the mainstream.
Typically, traditional manufacturing techniques and materials are used to produce the structural section of functional prosthetics. AM is often then implemented at the interface section by producing complex contours that fit perfect to the users’ anatomy improving comfort and fit. AM is also implemented on the external outer surface of prosthetics to produce life-like and organic outer shells that hide the mechanical nature of prosthetics. This also allows the wearer to fully customize their prosthetics to whatever design or style they prefer.

| Technology | Best suited for |
|---|---|
| FDM | Low cost solution for simple geometries. Very anisotropic making it unsuitable for most functional applications. |
| SLA | Very high level of detail. Parts are brittle so best suited for aesthetic applications. Parts have a smooth surface and are able to be painted. |
| SLS | Good strength and a high level of accuracy sees SLS often implemented at the interface section of functional prosthetics. The shape of the mating surface that is in contact with a user's anatomy is important for comfort and functionality. |
| Material jetting | Like SLA, best suited for aesthetic applications. Allows parts to be printed in full colour with a high level of detail. |
| Metal printing | Parts have good strength and complex design are able to be produced. Parts are generally very expensive. |
Hearing aids
Much to many people’s surprise hearing aids are one of the greatest success stories to come from the continued development of AM. Over 10,000,000 people are now wearing 3D printed hearing aids with 97% of all hearing aids globally now being created using AM. Not only has AM technology significantly reduced the cost of custom hearing aids when compared to traditional manufacturing but the ability to produce the complex and organic surfaces required for a hearing aid has reduced returns because of bad fit from 40% to 10%.

| Technology | Best suited for |
|---|---|
| SLA | The large majority of hearing aids are produced using SLA with the process very well established in industry. High level of detail allows for excellent customisation while the smooth surface improves comfort and fit. |
Limitations
Some of limitations of AM when applied to the medical industry include:
- While time to print parts is often much faster when compared to traditional manufacturing methods there is still significant time required for the conversion of scan data to produce a printable STL file. Because of this, for more urgent cases like trauma surgery, generic implants or medical devices may be a more desirable solution.
- While the purchase of a desktop FDM or SLA machine typically ranges from $1000 - $5000, high-end AM printers (SLS, material jetting and metal printing) range from $200,000 to $850,000. Materials for these AM technologies are also currently very expensive. Currently, for these technologies, the optimal solution is to get products made out of house.
- A sound understanding of each AM technology is critical and needs to be determined within the context of the desired outputs. Each technology has strengths and weaknesses and the variation in price to get parts made can be significant.
Case study - Sensor equipped neonatal models
Eindhoven’s University of Technology is home to PhD candidate and Healthcare Flagship Program participant, Mark Thielen, who is aiming to increase surgical and procedural success for neonatal patients. Using 3D printing and Protolabs Network, Mark has developed an optimised training experience using lifelike newborn models with functional organs capable of intelligent sensor feedback.

For surgeons and nurses, interacting with anatomical models is important to the success of surgeries and medical procedures. Within the neonatal field, it’s incredibly difficult to practice correctly with the current state of practice mannequins which lack the complexity and feel of a newborn patient. Mark’s research is to develop mannequins which have all their major internal organs functioning and equipped with sensors to monitor key measurements such as pressure, stress and impact during trial procedures (e.g CPR, intubation).
3D printing is utilized because of the vast materials available for testing and, most importantly, the organic shapes the technology is able to create. There are two key components to the mannequin: the ribcage/spine, which acts as the housing for the second component, the internal organs. The sheer complexity of human anatomy is very hard to recreate realistically with any other production method as well as increased cost and lead times.
Testing was initially done with various thermoplastic elastomers on a desktop FDM 3D printer to create the larger parts of the model such as the rib cage. After finalizing on a design, Selective Laser Sintering (SLS) was used because of the accuracy and dimensional freedom the technology offers.
To create the functional organs material jetting 3D printing was used to create molds. When compared to traditional manufacturing methods, 3D printed molds allowed for rapid design changes. Material jetting also allowed the combination of materials (rigid and flexible plastics) when creating the molds. A heart, for example, needed to have highly detailed working valves. Due to the extremely small sizes of neonatal organs, as well as their minuscule detail, the only way to create a mold for these parts was to 3D print them.

When the ribcage and organs are combined, Mark runs a fluid through the mannequin with two cameras and sensors installed, giving feedback on every part of the model throughout various trial procedures.
Mark’s research into the creation of hyper-realistic mannequins doesn’t stop at neonatal patients though, with there being potentially wider applications. He goes on to explain:
“I believe that developing and advancing what we started here can aid medical research in a broader scope. We could potentially create realistic patient models of other body parts to strengthen medical training for emergency procedures and pregnancies.”
The above case study was made possible by the D.search lab and Jasper Sterk who have both greatly contributed towards this research.